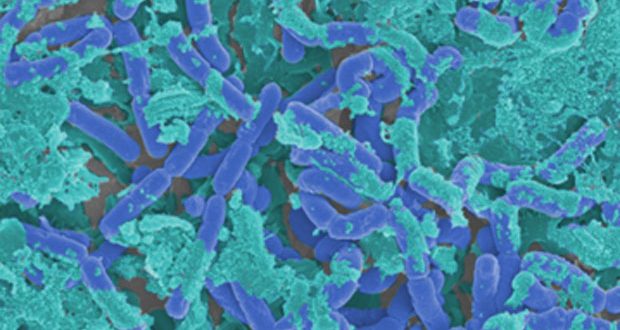
Healthcare providers increasingly find certain stubborn pathogens are a constant presence on particular wards. Despite diligent disinfection, certain Gram-negative or emerging pathogens such as persistent fungus Candida auris seem to create recurrent outbreaks with no clear cause. Emerging research shows that dry surface biofilms (DSBs) may be the culprits.[1],[2]
Recurrent outbreaks of Candida auris in hospital settings have caused ward closures, serious infections and death. It hit a neonatal unit in Venezuela, infiltrated through a hospital in Brooklyn and it closed an intensive care unit in a busy London Hospital for an incredible 11 days.[3],[4] Scientists are beginning to understand that superbugs, like Candida auris and MRSA, have a partner in crime – an emerging micro-organism, DSBs.
Prof Jean-Yves Maillard, Professor of Pharmaceutical Microbiology at Cardiff University and a world-leading expert on DSBs explained: “DSBs pose significant challenges in clinical settings because they protect organisms contained within them, they are difficult to eradicate and are invisible to the naked eye. Our research suggest that traditional disinfectants kill the free floating micro-organisms, but the DSBs provide a ‘life raft’ allowing the bugs to be protected from cleaning and disinfection. For the hospital this will mean that life-threatening superbug outbreaks (of Candida auris for example) can be very, very difficult to bring under control with traditional cleaning methods. Awareness of DSBs is low but it is key that hospital settings understand the impact of DSBs and adjust their infection prevention protocols accordingly.”
A study, led by Professor Maillard at the University of Cardiff, examined 61 surfaces that had already been disinfected: 60 of them were still harbouring DSBs (and more than half of those samples grew antibiotic-resistant micro-organisms).[5] Environmental DSBs are collections of micro-organisms which form a protective dry biofilm on a surface, which renders traditional chlorine-based disinfectants (routinely used in NHS hospitals) far less effective. It is thought that biofilm formation provides protection and nutrients for microorganisms, allowing them to survive in hostile environments. Investigators at Cardiff University identified only one disinfectant to completely prevent the biofilm from transferring to other surfaces and delayed regrowth of the biofilm for eight days, peracetic acid (3500 ppm).[6]
“Peracetic acid is a powerful oxidative disinfectant,” said Prof Maillard. “Unlike chlorine, peracetic acid isn’t inactivated by organic matter – making it a great candidate for tackling DSBs. This is likely why Peracetic Acid based product produced the highest reduction in viable organisms and were significantly more effective in biofilm eradication. It is important that we raise and educate IPC leads across the NHS not only on emerging antibiotic resistant superbugs, but how they work together with DSBs and when to use different cleaning protocols.”
Karen Wares, Clinical Director at GAMA Healthcare said: “At GAMA we focus our research on preventing infection, to help prevent and improve lives. New strategies to tackle the threat of DSBs, including the use of alternative products such as Peracetic Acid Wipes, are a critical part of hospital’s infection prevention strategy.”
Clinell Peracetic Acid Wipes (formerly known as Clinell Sporicidal Wipes) are proven to be more effective than chlorine against hard-to-kill organisms in real clinical environments.[7] They’re proven to reduce the total counts of aerobic and anaerobic organisms,[8] to be more effective at reducing persistent Gram-negative organisms and to reduce the incidence of C. difficile-associated disease by 72 per cent.[9] Deep-cleaning with peracetic acid has proven efficacy against certain organism and DSBs.
www.gamahealthcare.com/clinell-peracetic-acid-wipes
References:
[1] Ledwoch K, Maillard JY. Candida auris dry surface biofilm (DSB) for disinfectant efficacy testing. Materials (Basel). 2019;12(1):4-13. doi:10.3390/ma12010018
[2] Otter JA, Vickery K, Walker JT, et al. Surface-attached cells, biofilms and biocide susceptibility: Implications for hospital cleaning and disinfection. J Hosp Infect. 2015. doi:10.1016/j.jhin.2014.09.008
[4] https://www.telegraph.co.uk/news/2016/07/08/intensive-care-unit-closed-as-three-people-die-from-new-superbug/
[5] Ledwoch K, Dancer SJ, Otter JA, et al. Beware biofilm! Dry biofilms containing bacterial pathogens on multiple healthcare surfaces; a multi-centre study. J Hosp Infect. 2018;100(3):e47-e56. doi:10.1016/j.jhin.2018.06.028
[6] Ledwoch K, Magoga M, Williams D, Fabbri S, Walsh J, Maillard J-Y. Is a reduction in viability enough to determine biofilm susceptibility to a biocide? Infection Control and Hospital Epidemiology, 2021 Mar 2;1-7. doi: 10.1017/ice.2021.42.
[7]Siani H, Wesgate R, Maillard JY. Impact of antimicrobial wipes compared with hypochlorite solution on environmental surface contamination in a health care setting: A double-crossover study. Am J Infect Control. 2018;46(10):1180-1187.
[8] Siani H, Wesgate R, Maillard JY. Impact of antimicrobial wipes compared with hypochlorite solution on environmental surface contamination in a health care setting: A double-crossover study. Am J Infect Control. 2018;46(10):1180-1187.
[9] Carter Y, Barry D. Tackling C. difficile with environmental cleaning. Nurs Times. 2011;107(36):22-25.